Radiation Oncology
The scope of this interdisciplinary area is the integration of non-invasive imaging with radiation planning and biology-guided, individualized radiotherapy. To achieve this goal, NCT/UCC Dresden and NCT Heidelberg focus on the development of modern methods of radiotherapy and identification of new molecular therapy targets and predictive biomarkers for therapy response. The joint organization of both sites within the National Center for Radiation Research in Oncology (NCRO), the Helmholtz Program-oriented funding and recently also within the NCT has led to numerous collaborative and complementary initiatives in biological, physics, translational and clinical research. This also includes the preclinical evaluation and clinical introduction of dual-energy computer tomography (CT) for proton radiotherapy planning, the evaluation of magnet resonance-guided radiotherapy using linear accelerator technology, development of magnet resonance-guided proton therapy or the joint performance of clinical trials.
Research profile Dresden
In Dresden, research in radiation oncology focuses on
(1) the biological and clinical investigation of proton radiotherapy and the optimization of its physical precision and clinical application
(2) the evaluation of biological targets and mechanisms of new combined treatment schedules and the prediction of treatment effects for the development of personalized radiation treatment schedules.
Both areas involve the utilization of modern imaging methods, prediction of treatment effects and future adaptive radiotherapy schedules.
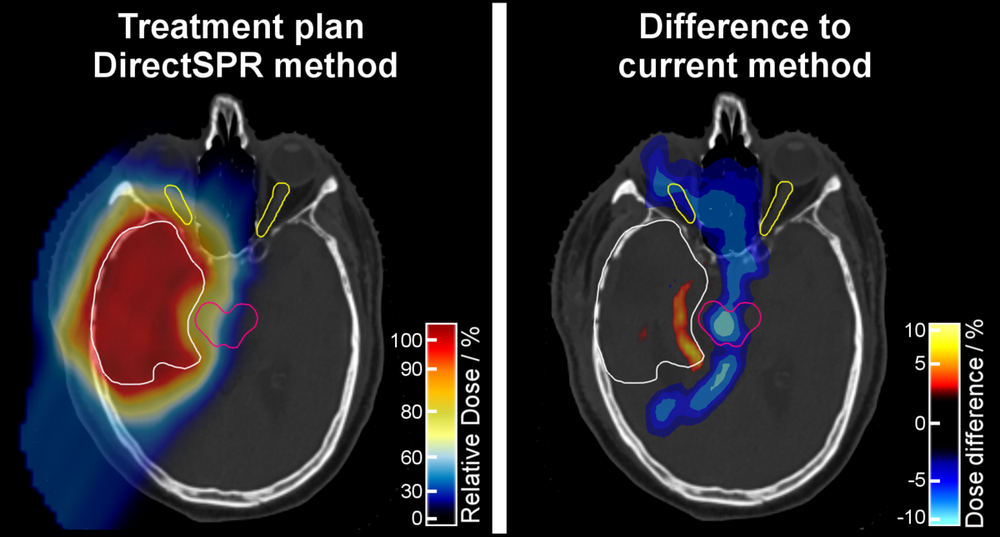
After five years of joint translational research in Dresden and Heidelberg, a novel method for particle therapy planning, based on information from a Dual-Energy CT scan of the patient, was introduced in clinical practice. With this so-called DirectSPR approach, the particle range in human tissue can be predicted more accurately and on an individual patient basis. The range accuracy, which has remained practically unchanged for more than 30 years, is thus for the first time significantly improved, resulting in a 35% reduction of the volume of irradiated healthy tissue surrounding the target volume. Therefore, DirectSPR increases the accuracy, safety and probably also the tolerability of particle therapy. This approach was developed as a medical device in intensive industrial collaboration and is available to particle therapy centres worldwide.
Wohlfahrt et al., Radiother Oncol 2017; Möhler et al., Phys Med Biol 2018; Peters et al., Radiother. Oncol. 2021.