PSMA-PET/MR-data for radiation treatment planning
Summary of the Project
In Germany, prostate cancer is the most common malignancy in men with an annual incidence of 64.000 and approx. 13.000 patients dying of metastatic disease.
In intermediate and non-metastatic high-risk prostate cancer patients, surgery (with adjuvant radiotherapy) or primary external beam radiotherapy (with anti-androgen treatment) is the therapy of choice. In external-beam irradiation, dose escalation of intermediate and high-risk prostate cancer has been shown to improve the outcome in patients with localized prostate cancer. However, the five-year biochemical relapse rate is still high.
Increasing the dose to the entire prostate is associated with an increase in severe acute and late toxicity. As local recurrences mainly occur in the primary tumor location, increasing the dose to the dominant intraprostatic lesion (DIL) to an ablative dose is expected to further improve local control rates. In this context, the accurate and precise identification and delineation of the DIL is of utmost importance.
As a unique and novel approach, the accuracy of DIL detection may be furthered combining multimodality magnetic resonance imaging (MRI) with positron emission tomography (PET) imaging using a PET tracer highly specific for prostate cancer, i.e., prostate-specific-membrane-antigen (PSMA). It is expected that combined PSMA-PET and MR imaging may yield complementary information for the characterization of intraprostatic lesions, ultimately more accurately and reliably identifying the DIL.
Our aim is to personalize radiotherapy of patients with prostate cancer by incorporation of combined PSMA-PET/MR-data into radiation treatment taking into account the accurate and precise localization and characterization of the DIL, as well as due possibly afore unknown (lymph node, bone) metastases.
Scientific Goals
- Optimize different PET/MR scanner protocols for use in prostate cancer patients.
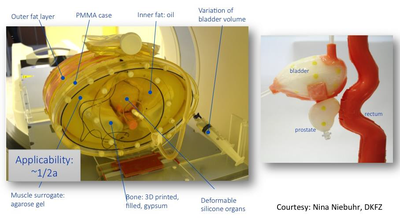
- Evaluation of geometric accuracy of PSMA-PET/MR-data in dependence of the diagnostic MR-sequences and PET-isotopes applied on the basis of a novel, for this specific study developed, modified anthropomorphic pelvis phantom.
- Comparison of the definition of the dominant intraprostatic lesion by PSMA-PET and/or MRI.
- Dosimetric comparison of the radiation treatment plans calculated with and without incorporation of PSMA-PET/MR-data in terms of dose to the target volume and to the organs at risk, boosting the dominant intraprostatic lesion.
- Assessment of the frequency of detecting afore unknown metastases and of the therapeutic consequences.
Figure 1. Abdominopelvic phantom to be adapted for the aims of this study.
Zegers CML, Hoebers FJP, van Elmpt W, Bons JA, Öllers MC, Troost EGC, Eekers D, Balmaekers L, Arts-Pechtold M, Mottaghy FM, Lambin P. Evaluation of tumor hypoxia during radiotherapy using [18F]HX4 PET imaging and blood biomarkers in patients with head and neck cancer. Eur J Nucl Med Mol Imag 2016;43(12):2139-46.
Jentsch C, Bergmann R, Brüchner K, Mosch B, Yaromina A, Krause M, Zips D, Troost E, Löck S, Kotzerke J, Steinbach J, Thames H, Baumann M, Beuthien-Baumann B. Impact of pre- and early per-treatment FDG-PET based dose-escalation on local tumour control in fractionated irradiated FaDu xenograft tumours. Radiother Oncol 121:447-452, 2016.
Troost EGC, Thorwarth D, Oyen WJG. Imaging-based treatment adaptation in radiation oncology. J Nucl Med 2015;56(12):1922-1929.
Grootjans W, de Geus-Oei L-F, Troost EGC, Visser EP, Oyen WJG, Bussink J. PET in the management of locally advanced and metastatic NSCLC. Nature Rev Clin Oncol 2015;12:395-407.
Schramm G, Maus J, Hofheinz F, Petr J, Lougovski A, Beuthien-Baumann B, Oehme L, Platzek I, van den Hoff J. Correction of quantification errors in pelvic and spinal lesions caused by ignoring higher photon attenuation of bone in [18F]NaF PET/MR. Med Phys. 42:6468-76, 2015.
Trani D, Yaromina A, Dubois L, Granzier M, Peeters S, Biemans R, Nalbantov G, Lieuwes N, Reniers B, Troost EGC, Verhaegen F, Lambin P. Pre-clinical assessment of efficacy of dose painting based on intratumoral FDG-PET uptake. Clin Canc Res 2015;21:5511-5518.
Platzek I, Beuthien-Baumann B, Schneider M, Gudziol V, Kitzler H, Langner J, Schramm G, Laniado M, Kotzerke J, van den Hoff J. FDG PET/MR for lymph node staging in head and neck cancer. Eur J Radiol. 83:1163-8, 2014.
Schramm G, Beuthien-Baumann B, Hofheinz F, Langner J, Petr J, Platzek I, Steinbach J, Kotzerke J, van den Hoff J. Quantitative accuracy of attenuation correction in the Philips Ingenuity TF whole body PET/MR system: a direct Page 24/27 comparison with transmission-based attenuation correction. Magnetic Resonance Materials in Physics, Biology and Medicine 26: 115-126, 2013.
Platzek I, Beuthien-Baumann B, Schneider M, Gudziol V, Langner J, Brüning E, Laniado M, Kotzerke J, van den Hoff J. Combined PET/MRI system in Head and Neck Cancer: Initial Experience. Eur J Nucl Med Mol Imaging 40:6-11, 2013.
Contact
Prof. Dr. med. Dr. Esther Troost
Klinik und Poliklinik für Strahlentherapie und Radioonkologie, Universitätsklinikum Carl Gustav; Institut für Radioonkologie - OncoRay, HZDR
Phone: +49 351 458 – 5414
Email: esther.troost(at)uniklinikum-dresden.de
Dr. med. Bettina Beuthien-Baumann
Abteilung Radiologie, DKFZ
Phone: +49 6221 42 – 3202
Email: b.beuthien-baumann(at)dkfz.de
Dr. med. Stefan Körber
Klinik für Radioonkologie, Universitätsklinikum Heidelberg
Phone: +49 6221 56 36589
Email: stefan.koerber(at)med.uni-heidelberg.de
Prof. Dr. med. Jörg Kotzerke
Klinik und Poliklinik für Nuklearmedizin, Universitätsklinikum Carl Gustav Carus
Phone: +49 351 458 4160
Email: joerg.kotzerke(at)uniklinikum-dresden.de
Dr. rer. nat. Asja Pfaffenberger
Abteilung Medizinische Physik in der Strahlentherapie, DKFZ
Phone: +49 6221 42 3483
Email: a.pfaffenberger(at)dkfz.de
Dr.-Ing. Aswin Hoffmann
Klinik und Poliklinik für Strahlentherapie und Radioonkologie, Universitätsklinikum Carl Gustav; Institut für Radioonkologie - OncoRay, HZDR
Phone: +49 351 458 – 3932
Email: aswin.hoffmann(at)uniklinikum-dresden.de