Institute of Radiooncology – OncoRay
The researchers of the HZDR Institute of Radiooncology – OncoRay work in different groups at the umbrella research platform OncoRay. The focus of activities of the OncoRay – National Center for Radiation Research in Oncology is translational research, which means that lab results should reach the patient as quickly as possible. OncoRay researchers thus get together with physicians from the Department of Radiotherapy and Radiooncology at Dresden University Hospital to conduct clinical studies examining promising research results. Furthermore, clinician scientists who work as physicians and researchers build a natural bridge between clinic and lab. Often, other hospitals, research groups and industrial partners are also involved on both a national and international level.
The OncoRay Center is an umbrella research platform, assembling 80 researchers from the three operating institutions: the University Hospital Carl Gustav Carus Dresden, the Carl Gustav Carus Faculty of Medicine at TU Dresden and the Helmholtz-Zentrum Dresden-Rossendorf. At OncoRay, they work in cross-disciplinary programs with focuses on medicine, physics, biology and information science.
Main fields of research are (selection):
- Biologically individualized radiotherapy including preclinical biomarker development
- Modeling of treatment effects for individualized patient selection for particle therapy and different beam qualities
- Image-guided radiotherapy
- Technological optimization of proton therapy including laser-accelerated particle radiotherapy
- Combined treatments, e.g. with targeted therapies, preclinical and clinical
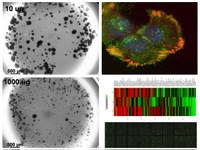
Right: immunofluorescence of integrins in tumor cells; transcriptome and proteome analyses in tumor cells after treatment.
Krause M, Dubrovska A, Linge A, Baumann M: Cancer stem cells: Radioresistance, prediction of radiotherapy outcome and specific targets for combined treatments. Adv Drug Deliv Rev 2017, 109:63-73
Linge A, Löck S, Gudziol V, Nowak A, Lohaus F, von Neubeck C, Jütz M, Abdollahi A, Debus J, Tinhofer I, Budach V, Sak A, Stuschke M, Balermpas P, Rödel C, Avlar M, Grosu AL, Bayer C, Belka C, Pigorsch S, Combs SE, Welz S, Zips D, Buchholz F, Aust DE, Baretton GB, Thames HD, Dubrovska A, Alsner J, Overgaard J, Baumann M, Krause M; DKTK-ROG. Low Cancer Stem Cell Marker Expression and Low Hypoxia Identify Good Prognosis Subgroups in HPV(-) HNSCC after Postoperative Radiochemotherapy: A Multicenter Study of the DKTK-ROG. Clinical Cancer Research (2016) 22(11):2639-49
Baumann M, Krause M, Overgaard J, Debus J, Bentzen SM, Daartz J, Richter C, Zips D, Bortfeld T. Radiation oncology in the era of precision medicine. Nature Reviews Cancer (2016) 16(4):234-49
Richter C, Pausch G, Barczyk S, Priegnitz M, Keitz I, Thiele J, Smeets J, Vander Stappen F, Bombelli L, Fiorini C, Hotoiu L, Perali I, Prieels D, Enghardt W, Baumann M.: First clinical application of a prompt gamma based in vivo proton range verification system. Radiother Oncol (2016) 118(2):232-7
Eke I, Zscheppang K, Dickreuter E, Hickmann L, Mazzeo E, Unger K, Krause M, Cordes N. Simultaneous β1 integrin-EGFR targeting and radiosensitization of human head and neck cancer. Journal of the National Cancer Institute (2015) 5;107(2)


